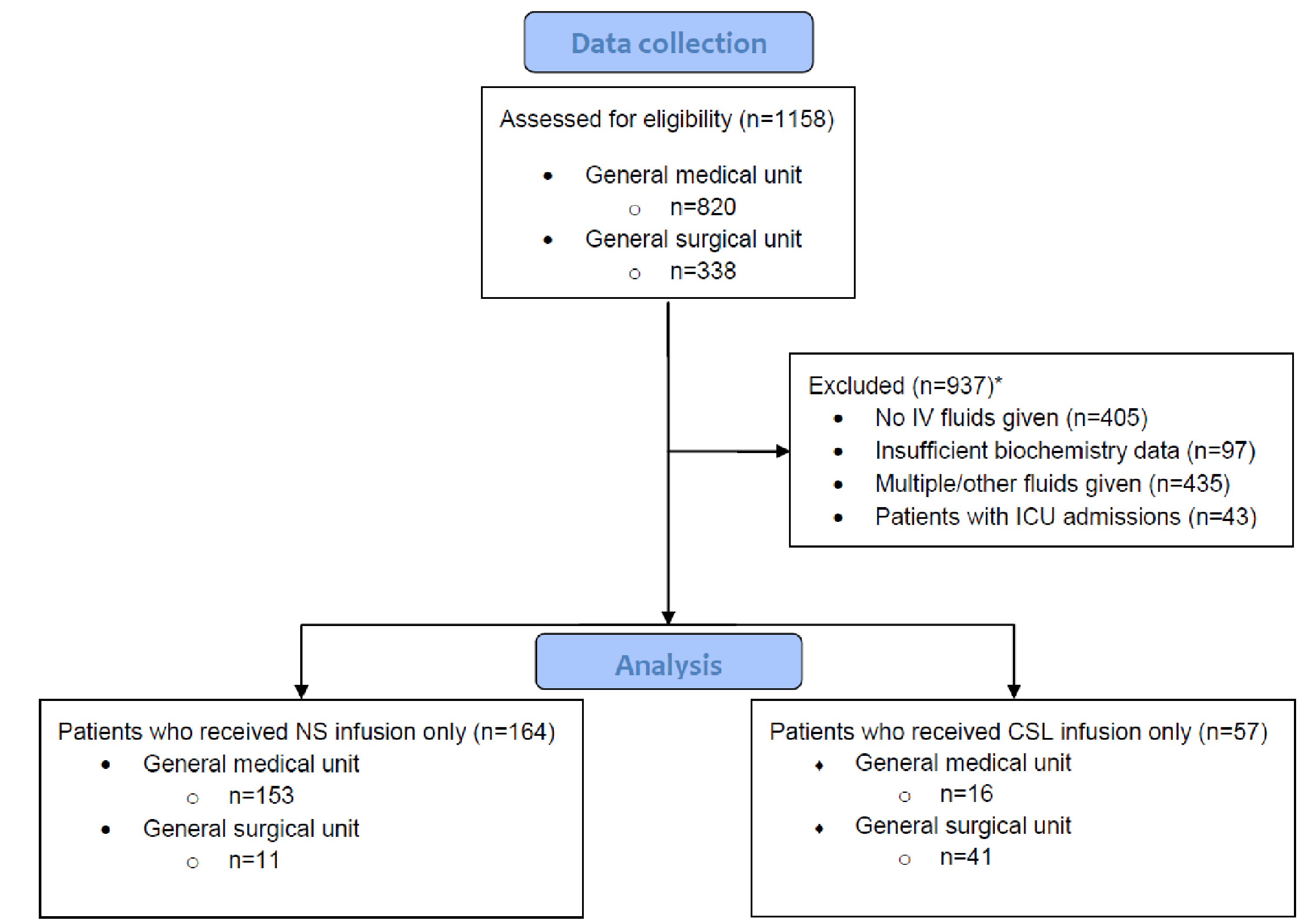
Figure 1. Criteria used for exclusion to obtain list of patients for final analysis. *Number of patients satisfying each exclusion criteria overlapped with other criteria. In total, there were 937 patients excluded from this study. CSL: compound sodium lactate; ICU: intensive care unit; IV: intravenous; NS: normal saline.