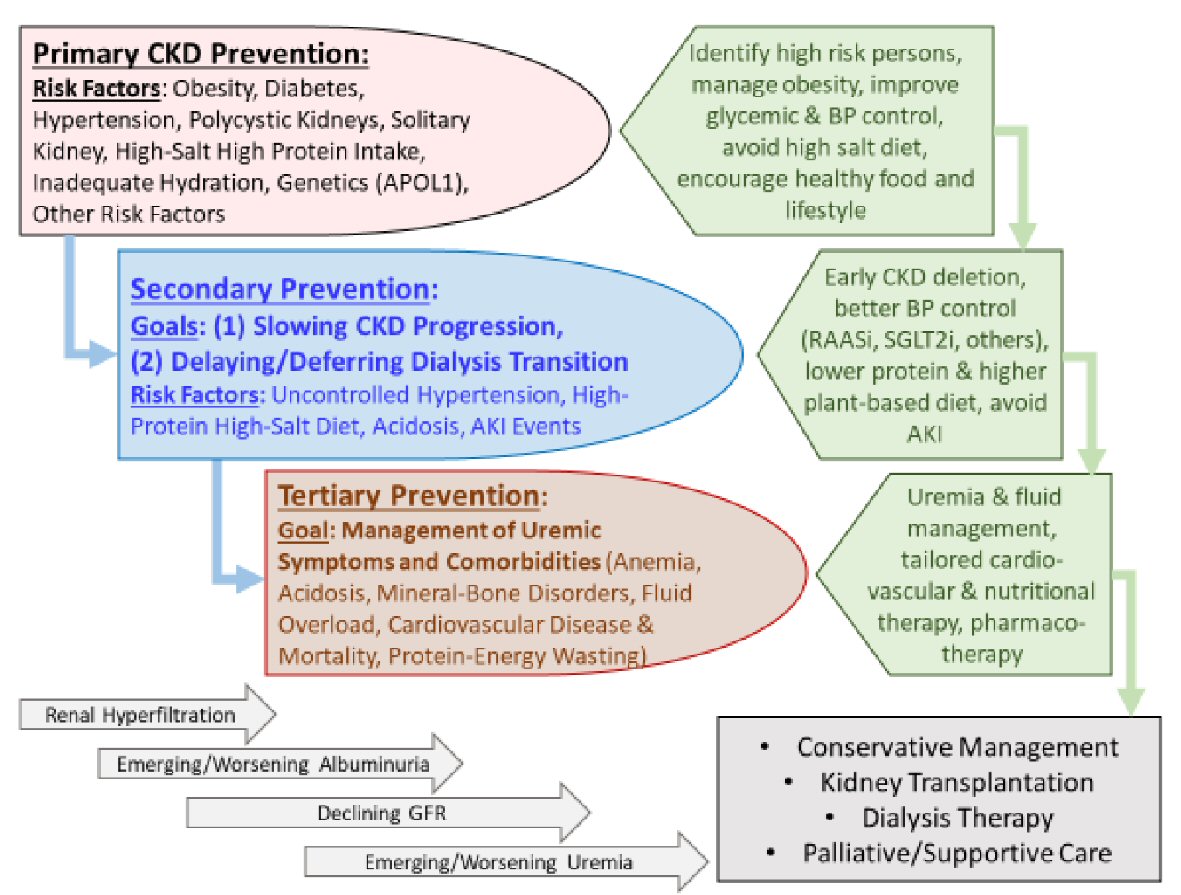
Figure 1. Overview of the preventive measures in chronic kidney disease (CKD) to highlight the similarities and distinctions pertaining to primary, secondary, and tertiary preventive measures and their intended goals.
| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website http://www.wjnu.org |
Review
Volume 9, Number 1, March 2020, pages 1-10
Kidney Health for Everyone Everywhere: From Prevention to Detection and Equitable Access to Care
Figure
Table
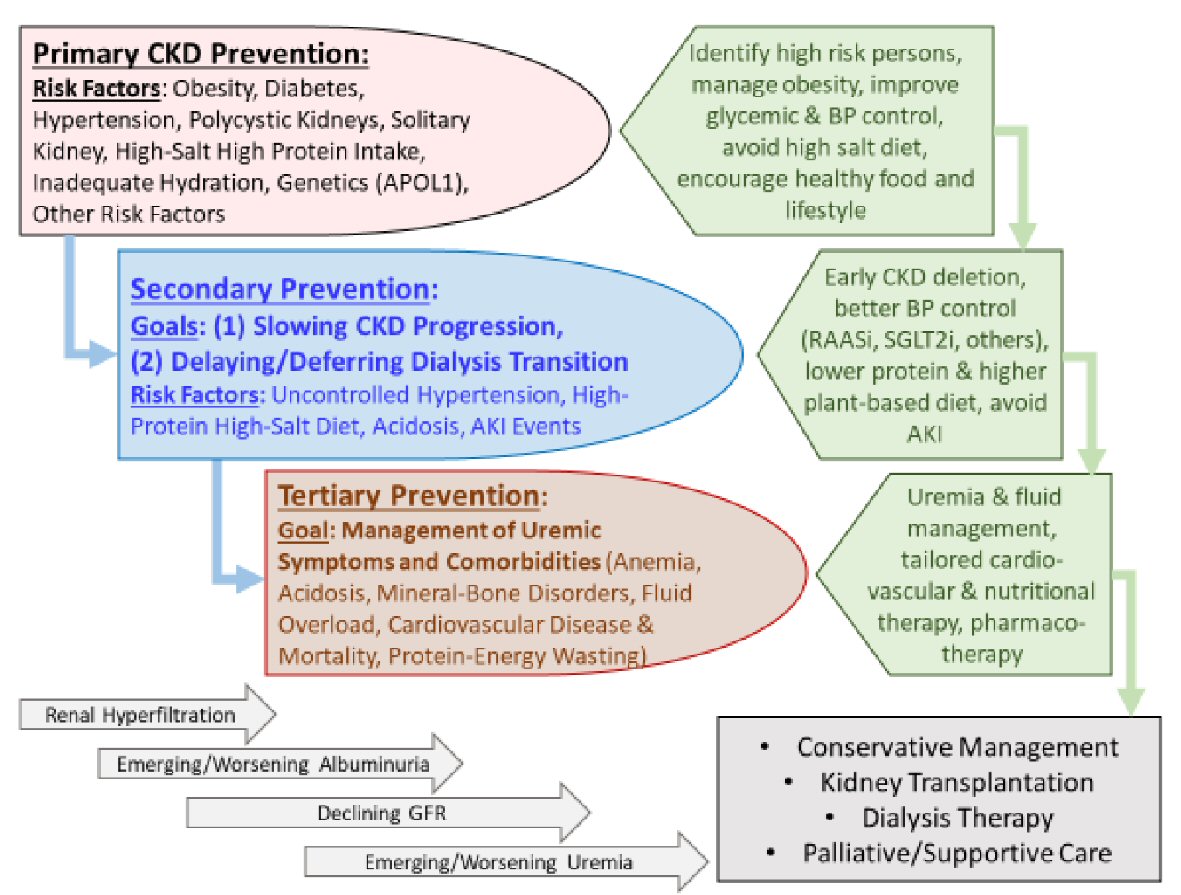
| Risk factorsa | Contribution to de novo CKD | Contribution to CKD progression |
|---|---|---|
| aMany of these risk factors contribute to both de novo CKD and its faster progression and hence are relevant to both primary and secondary prevention. ACEI: angiotensin converting enzyme inhibitor; AIN: acute interstitial nephritis; AKI: acute kidney injury; APOL1: apolipoprotein 1; ATN: acute tubular necrosis: BPH: benign prostate hypertrophy; CKD: chronic kidney disease; CNI: calcineurin inhibitor; GN: glomerulonephritis; NASH: non-alcoholic steatohepatitis; NSAID: non-steroidal anti-inflammatory drug; PPI: proton pump inhibitor. | ||
| Diabetes mellitus | About 50% of all CKDs | |
| Hypertension | About 25% of all CKDs | |
| Obesity | 10-20% | |
| Age | Seen with advancing age, especially in the setting of comorbid conditions. | Some suggests that older CKD patients may have slower progression. |
| Race, genetics and other hereditary factors | Common among those with African American ancestors. | |
| APOL1 gene | ||
| Hereditary nephritis (Alport’s) | ||
| Acute glomerulonephritis | < 10% | Recurrent GN or exacerbation of proteinuria |
| Post-infectious GN | ||
| Rapidly progressive GN | ||
| Polycystic kidney disorders | < 10%, family history of cystic kidney disorders | |
| Acute kidney injury (AKI) | Repeated AKI bouts can cause CKD | Repeated AKI bouts can accelerate CKD progression. |
| Acute tubular necrosis (ATN) | ||
| Acute interstitial nephritis (AIN) | ||
| Autoimmune disorders | ||
| Lupus erythematosus | ||
| Other connective tissue disorders | ||
| Pharmacologic | Variable, e.g. in Taiwan, Chinese, herb nephropathy may be an important contributor. | |
| Medications causing interstitial nephritides (NSAIDS, CNI, chemotherapy, PPI, etc) or ATN (aminoglycosides) | ||
| Herbs and herbal medication | ||
| Environmental | Rare | |
| Heavy metal exposure | ||
| Acquired or congenital solitary kidney | ||
| Cancer, donor or traumatic nephrectomy | ||
| Congenital solitary kidney, unilateral atrophic kidney | ||
| Acquired urinary tract disorders and obstructive nephropathy | BPH in men | |
| Gynecological cancers in women | ||
| Congenital anomalies of the kidney and urinary tract | Mostly in children and young adults | |
| Inadequate fluid intake | Unknown risk, but high prevalence is suspected in Central America. | Whereas in earlier CKD stages adequate hydration is important to avoid pre-renal AKI bouts, higher fluid intake in more advanced CKD may increase the risk of hyponatremia. |
| Mesoamerican nephropathy | ||
| Others | ||
| High protein intake | Unknown risk, recent data suggest higher CKD risk or faster CKD progression with high protein diet, in particular from animal sources. | Higher protein intake can accelerate the rate of CKD progression. |
| Cardiovascular diseases (cardiorenal) | Ischemic nephropathy | |
| Liver disease (hepatorenal) | NASH cirrhosis, viral hepatitis | |