| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website https://www.wjnu.org |
Original Article
Volume 9, Number 2, December 2020, pages 35-39
Outcome of Percutaneous Nephrolithotomy in a Tertiary Care Center in North Karnataka
Sushant Deolea, Shridhar C. Ghaganeb, Priyeshkumar Patela, R.B. Nerlia, c, Shashank D. Patila, Neeraj S. Dixitb
aDepartment of Urology, JN Medical College, KLE Academy of Higher Education and Research, JNMC Campus, Belagavi, Karnataka 590010, India
bUrinary Biomarkers Research Centre, Department of Urology, KLES Kidney Foundation, KLES Dr. Prabhakar Kore Hospital and Medical Research Center, Nehru Nagar, Belagavi, Karnataka 590010, India
cCorresponding Author: R. B. Nerli, Department of Urology, JN Medical College, KLE Academy of Higher Education and Research, JNMC Campus, Belagavi, Karnataka 590010, India
Manuscript submitted July 7, 2020, accepted September 9, 2020, published online November 25, 2020
Short title: PCNL for Renal Stones
doi: https://doi.org/10.14740/wjnu412
| Abstract | ▴Top |
Background: The study aims to evaluate the results of percutaneous nephrolithotomy (PCNL) in terms of patient and stone characteristics, stone clearance, and complications in the management of renal stones in our hospital.
Methods: We retrospectively analysed the outcomes of 320 patients who underwent PCNL between December 2017 and December 2019. Data analysed included patient demographics, investigations, site of calyceal puncture, operative time, number of tracts, stone-free rates (SFRs), hospital stay, and complications.
Results: Out of 320 patients, 246 (76.87%) were males and 74 (23.13%) were females with male to female ratio 3.32:1. The mean age was 36.4 ± 11.8 years (range: 18 - 74). The mean operative time was 120 ± 40 min (± standard deviation (SD)). The radiation exposure time ranged from 1 min 30 s to 30 min with a mean (± SD) of 8.2 min (± 3.6). The mean hospital stay duration was 3.2 ± 1.6 days. Complete stone clearance was 92.18% whereas SFRs defined by no identifiable stone on plain radiograph or ultrasound or residual fragments < 5 mm was 95.93%. The complication rate was 11.8%.
Conclusions: PCNL is the standard treatment for large renal stones > 2 cm. Stone burden, type of stone, access puncture, and several tracts, and operative time significantly affect SFRs. With the miniaturization of instruments and the development of different lithotripsy techniques, PCNL remains a very good treatment for large renal stones with acceptable complication rates.
Keywords: Percutaneous nephrolithotomy; Stone-free rates; Flexible nephroscope; Staghorn stone
| Introduction | ▴Top |
Urolithiasis and its treatment constitute almost 30% of the workload in the urology department [1]. The minimally invasive technique for the treatment of renal stones, i.e., percutaneous nephrolithotomy (PCNL) was first described by Fernstrom and Johansson [2] in 1976 and is standard of care for renal calculus > 2 cm in size, complex (staghorn stone), extracorporeal shock wave lithotripsy (ESWL) refractory and lower pole calculus. Other indications are calyceal diverticular stone, associated with anatomical anomaly (horseshoe kidney, ectopic kidney) [3]. There have been tremendous developments in PCNL techniques like miniaturization of instruments to reduce the tract size, shift of puncture from fluoroscopy-guided to ultrasound-guided, improvements in tract dilatation like balloon dilatation, single-step dilatation. And the advancement in lithotripsy techniques from electro-hydraulic, ballistic, ultrasound to Laser has been tremendous. Developments in imaging from plain radiographs, ultrasound to computed tomography has helped surgeons to better plan the procedure. Scoring systems like STONE nephrolithometry score, Guy’s stone score helps in pre-operative assessment of outcome of PCNL [4, 5]. Staghorn morphometry is also a prognostic tool to predict the outcome of PCNL [6].
| Materials and Methods | ▴Top |
We retrospectively analyzed the records of 320 patients who underwent PCNL between December 2017 and December 2019 in the tertiary care center. The patients underwent a detailed history and physical examination. Laboratory investigations included complete blood count, kidney function tests, blood sugars, coagulation profile, and urine analysis. All patients diagnosed to have renal stone on ultrasonography or plain radiograph of kidney, ureter, and bladder (KUB) were further evaluated with non-contrast computed tomography (CT) KUB. Anesthesia risk assessment and fitness for surgery were done. Patients were posted for surgery only after a sterile urine culture report and those who had urinary tract infection (UTI) were treated with antibiotics 1 week before surgery and after confirming sterile culture report. The workflow diagram of the study was presented (Fig. 1). The study was approved by institutional review board and complied with ethical standards.
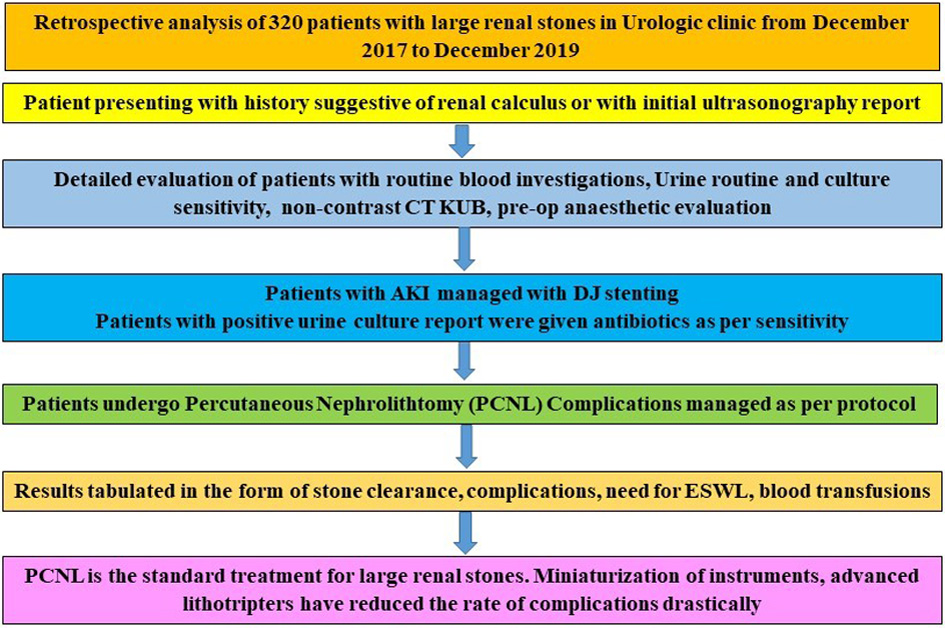 Click for large image | Figure 1. The workflow diagram of the study. PCNL: percutaneous nephrolithotomy; CT: computed tomography; KUB: kidney, ureter, and bladder; AKI: acute kidney injury; ESWL: extracorporeal shock wave lithotripsy. |
PCNL technique
All procedures were done under general anesthesia. Six-Fr ureteric catheter was placed cystoscopically in the renal collecting system under fluoroscopic guidance. After the patient was put in a prone position, retrograde pyelography was done to delineate the pelvicalyceal system and plan puncture. Target calyx was punctured with an 18-gauge needle under fluoroscopic guidance using either Bull’s eye technique or triangulation technique. After confirming puncture, Terumo guidewire was passed and directed into ureter. In cases where multiple tracts were expected, multiple punctures were made, and wire passed through them. The tract was dilated initially with fascial dilators till 10 Fr and then serially dilated with Alkens telescopic dilators over central guide rod and fluoroscopy up to 24 or 30 Fr. An appropriately sized Amplatz sheath was placed. Rigid nephroscope (Storz; Germany-24/30 Fr) was passed, stones visualized and fragmented with pneumatic lithotripsy (EMS).
The stone fragments were retrieved using a bi-radiate grasper. Six-Fr double-J stent was passed in all cases as it is our departmental protocol. Nephrostomy was kept when necessary (18 - 22 Fr Nelaton catheter) for 24 - 48 h. On the first post-operative day, ultrasonography, X-ray KUB, and hemoglobin level were routinely done. Nephrostomy tube was removed on the first or second postoperative day irrespective of stone-free rates (SFRs) as we don’t proceed with second look PCNL. The SFR was defined by no identifiable stone on ultrasonography (USG) or X-ray or with clinically insignificant residual fragment < 5 mm. Patients with residual stones were planned to ESWL at a later date. Complications were graded as per Clavien classification and its modifications for percutaneous procedures.
| Results | ▴Top |
During the period of study, 320 patients underwent PCNL. The patient demographics and stone characteristics are as shown in (Table 1). Majority of the patients (n = 241, 75.31%) presented with flank pain of variable duration. Other symptoms were hematuria (n = 52, 16.25%), fever with urinary tract infection (n = 21, 6.56%) and acute kidney injury (AKI) (n = 11, 3.43%). Out of 11 patients with AKI, 7 (63.63%) were managed conservatively with intravenous (IV) antibiotics, 3 (27.27%) patients required double-J stenting, and 1 (9.09%) patient had Percutaneous nephrostomy tube placement. Serum creatinine levels came to normal in 9 patients and 2 patients had elevated creatinine levels after 2 weeks. Fifty patients (15.62%) had a history of previous stone disease out of which 5 (10%) underwent open surgery, 26 (52%) underwent ureteroscopy, 9 (18%) underwent ESWL and 10 (20%) had a history of PCNL. Most procedures were done using a single tract of 288 cases (90%), two tracts in 29 cases (9.06%), and three tracts in 3 cases (0.94%). Table 2 shows access sites and distribution in detail.
 Click to view | Table 1. Patient Demographics and Stone Characteristics (N = 320) |
 Click to view | Table 2. Number and Distribution of Access Puncture |
Nephrostomy tube in the form of a Nelaton catheter was kept in 300 cases (93.75%). The mean operative (± standard deviation (SD)) time was 120 min (± 40). The radiation exposure time ranged from 1 min 30 s to 30 min with a mean (± SD) of 8.2 min (± 3.6). The mean hospital stay duration was 3.2 ± 1.6 days. The SFRs concerning stone size are shown in (Table 3). Complete clearance was observed in 295 cases (92.18%). The highest clearance rate was observed when the stone was a single mass with as high as 96% which reduced to as low as 70% when the stone was complete staghorn. Only the patients with > 5 mm residual fragments were subjected to ESWL. All 13 patients were rendered stone-free after post-ESWL, nine of which needed only one sitting of ESWL while four required ESWL twice with a gap of 15 days.
 Click to view | Table 3. Stone Clearance After PCNL |
Complications occurred in 38 cases (11.8%) out of which six cases had two complications. Fever was observed in 15 cases whereas bleeding (intra-operative and post-operative) occurred in 22 cases out of which 20 cases (6.25%) required blood transfusions. None of the patients required angioembolization or nephrectomy for bleeding complications. Nephrostomy site urine leak was observed in 8 cases which were conservatively managed by watchful waiting. Fever was managed by antipyretics and occasionally by higher antibiotics. One patient had colonic injury which was identified post-operatively after the removal of a nephrostomy tube which was managed by colostomy after failure of conservative management.
| Discussion | ▴Top |
Stone disease is highly prevalent in India and is almost 30% of the caseload in the urology department. Various treatment modalities like ESWL, retrograde intrarenal surgery (RIRS), and PCNL are available. PCNL has become the standard of treatment for renal stones > 2 cm due to high success rates and acceptable morbidity [7]. There has been a significant decline in open surgery for urolithiasis but in some developing countries the number is still high [8]. The male to female ratio in our study is 3.32:1.
CT scan for pre-operative evaluation was done in 100% of the patients in our study. CT is the imaging modality of choice before PCNL for measuring stone size, location, Hounsfield units (HU), for various scoring systems, predicting stone clearance, planning access to the collecting system, and predicting complications [9].
The complete clearance of stone in the present study was 92.18% with 3.75% cases having clinically insignificant residual fragments (< 5 mm). The SFR was defined as no identifiable stone on USG and X-ray or clinically insignificant residual stone (CIRF). So, the SFR in the present study was 95.93%. This is similar to the previously reported study which showed 93% complete clearance and SFR was 98% when CIRF were included [10].
All the patients having residual fragments > 5 mm were rendered stone-free after combination therapy with ESWL. However, a CT scan was not done to confirm SFRs, so the probability of SFRs being lower cannot be ruled out. In a multicentre study, higher body mass index (BMI) was associated with a risk of bleeding, less SFRs, and prolonged operative time [11]. But the present study did not observe high BMI with decreased SFR. Similar findings were reported by Kuntz et al [12] and Tomaszewski et al [13].
In a study to evaluate SFR using stone surface area and stone type, Turna et al [14] observed that increased surface area and stone type lowered the SFRs. This was similar to the present study that SFR reduced as the surface area increased with maximum SFR for single stone (96%) to lowest SFR for complete staghorn stone (70%). Anastasiadis et al [15] in their study on the impact of stone density on outcomes in PCNL found that the highest success rates were found when HU of the stone was 1,250 and that the success rates reduced when the density of the stone decreased or increased beyond 1,250 HU. However, in the present study, there was no significant difference between the stone density and SFR.
In 90% (n = 288) of the cases, PCNL was done through a single tract, 9.06% (n = 29) required two tracts while only 0.94% (n = 3) required three tracts. With the advent of flexible nephroscope, superior calyceal puncture improves the clearance of all calyceal stones [16]. The improved stone clearance with single access for large and complex stones was also reported by Shalaby et al [17]. However, by a study by Desai and Hegarty [18], they found that creatinine values increased significantly when multiple tracts were used. However recent studies show that there is no significant renal damage with multiple tracts which was confirmed by GFR estimation [19]. However multiple tracts were associated with increased intraoperative bleeding and increased need for blood transfusion.
Gaining percutaneous access was done by fluoroscopy in 100% cases in the present study by using either Bull’s eye or triangulation technique [20]. However, to reduce radiation exposure, the use of ultrasonography to gain percutaneous access in real-time has gained popularity as it is inexpensive and readily available [21]. Also, its advantage in pregnancy, ectopic kidney, and horseshoe kidney has made ultrasonography a much-needed armamentarium for urologists.
In the present study the mean operative time was 120 ± 40 min which as per Clinical Research Office of the Endourological Society (CROES) study comes under long time group [22]. Longer operative time increases anesthesia risks and respiratory complications [23], increased blood loss, and the need for transfusions [24]. The factors which affect the operative time are stone load and stone type, complexity of collecting system, obesity, and expertise of the surgeon [25].
There was a study showing nephrostomy tube placement reduced the complication rates without any effect on hospital stay and need of analgesia [26]. Nephrostomy in the present study was placed in 300 cases (93.75%) and found no significant difference between nephrostomy placement and complication rates. In the present study, stone burden, and the stone type, stone density, operative time, and number of access points affected the SFRs. This was supported by the study by Abdelhafez et al [27]. A complication rate of 20.5% was reported by the CROES PCNL global study group [3]. Another study reported a complication rate of 48.2% [28]. The present study reports a complication rate of 11.8%.
With developments in technology, ultrasound-guided puncture, miniaturized instruments, use of scoring systems, flexible nephroscope, and laser lithotripsy devices, the Stone free rates can be improved, and the complication rates can be brought down. All the above mentioned were not applied and have limitations in our study.
Conclusions
PCNL is the standard of care of renal stones > 2 cm with acceptable complication rates and morbidity. With the advancement, SFR can be improved and complications brought down further.
Acknowledgments
The authors highly appreciate the support rendered by the patient and nursing staff during the course of this study.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that they have no competing interest.
Informed Consent
All the patients had given written informed consent prior to being the part of this study.
Author Contributions
SD contributed to conceptualization of the study, experiments and writing the original manuscript. SCG did statistical analysis, reviewed and edited the manuscript. PP and SDP collected the data of the patients. RBN supervised the study and revised the manuscript. NSD did public relation support between the patients. All the authors reviewed and approved the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Pearle MS, Calhoun EA, Curhan GC, Urologic Diseases of America P. Urologic diseases in America project: urolithiasis. J Urol. 2005;173(3):848-857.
doi pubmed - Fernstrom I, Johansson B. Percutaneous pyelolithotomy. A new extraction technique. Scand J Urol Nephrol. 1976;10(3):257-259.
doi pubmed - de la Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpa R, Tefekli A, et al. The Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study: indications, complications, and outcomes in 5803 patients. J Endourol. 2011;25(1):11-17.
doi pubmed - Thomas K, Smith NC, Hegarty N, Glass JM. The Guy's stone score—grading the complexity of percutaneous nephrolithotomy procedures. Urology. 2011;78(2):277-281.
doi pubmed - Smith A, Averch TD, Shahrour K, Opondo D, Daels FP, Labate G, Turna B, et al. A nephrolithometric nomogram to predict treatment success of percutaneous nephrolithotomy. J Urol. 2013;190(1):149-156.
doi pubmed - Mishra S, Sabnis RB, Desai MR. Percutaneous nephrolithotomy monotherapy for staghorn: paradigm shift for 'staghorn morphometry' based clinical classification. Curr Opin Urol. 2012;22(2):148-153.
doi pubmed - Turk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, Seitz C. EAU guidelines on urolithiasis. Arnhem: European Association of Urology. 2010.
- El-Husseiny T, Buchholz N. The role of open stone surgery. Arab J Urol. 2012;10(3):284-288.
doi pubmed - Kumsar S, Aydemir H, Halis F, Kose O, Gokce A, Adsan O. Value of preoperative stone scoring systems in predicting the results of percutaneous nephrolithotomy. Cent European J Urol. 2015;68(3):353-357.
doi pubmed - Chibber PJ. Percutaneous nephrolithotomy for large and staghorn calculi. J Endourol. 1993;7(4):293-295.
doi pubmed - Fuller A, Razvi H, Denstedt JD, Nott L, Pearle M, Cauda F, Bolton D, et al. The CROES percutaneous nephrolithotomy global study: the influence of body mass index on outcome. J Urol 2012;188(1):138-144.
doi pubmed - Kuntz NJ, Neisius A, Astroza GM, Tsivian M, Iqbal MW, Youssef R, Ferrandino MN, et al. Does body mass index impact the outcomes of tubeless percutaneous nephrolithotomy? BJU Int. 2014;114(3):404-411.
doi pubmed - Tomaszewski JJ, Smaldone MC, Schuster T, Jackman SV, Averch TD. Outcomes of percutaneous nephrolithotomy stratified by body mass index. J Endourol. 2010;24(4):547-550.
doi pubmed - Turna B, Umul M, Demiryoguran S, Altay B, Nazli O. How do increasing stone surface area and stone configuration affect overall outcome of percutaneous nephrolithotomy? J Endourol. 2007;21(1):34-43.
doi pubmed - Anastasiadis A, Onal B, Modi P, Turna B, Duvdevani M, Timoney A, Wolf JS, Jr., et al. Impact of stone density on outcomes in percutaneous nephrolithotomy (PCNL): an analysis of the clinical research office of the endourological society (CROES) pcnl global study database. Scand J Urol. 2013;47(6):509-514.
doi pubmed - Beaghler MA, Poon MW, Dushinski JW, Lingeman JE. Expanding role of flexible nephroscopy in the upper urinary tract. J Endourol. 1999;13(2):93-97.
doi pubmed - Shalaby MM, Abdalla MA, Aboul-Ella HA, El-Haggagy AM, Abd-Elsayed AA. Single puncture percutaneous nephrolithomy for management of complex renal stones. BMC Res Notes. 2009;2:62.
doi pubmed - Hegarty NJ, Desai MM. Percutaneous nephrolithotomy requiring multiple tracts: comparison of morbidity with single-tract procedures. J Endourol. 2006;20(10):753-760.
doi pubmed - Handa RK, Evan AP, Willis LR, Johnson CD, Connors BA, Gao S, Lingeman JE, et al. Renal functional effects of multiple-tract percutaneous access. J Endourol. 2009;23(12):1951-1956.
doi pubmed - Bernardo ON. Percutaneous renal access under fluoroscopic control. In: Smith AD, Badlani GH, Preminger GM, Kavoussi LR, eds, Smith's Textbook of Endourology, 3rd edn. West Sussex: Wiley-Blackwell Publishing Ltd., 2012: p. 180-188.
doi - Chi T, Masic S, Li J, Usawachintachit M. Ultrasound guidance for renal tract access and dilation reduces radiation exposure during percutaneous nephrolithotomy. Adv Urol. 2016;2016:3840697.
doi pubmed - Labate G, Modi P, Timoney A, Cormio L, Zhang X, Louie M, Grabe M, et al. The percutaneous nephrolithotomy global study: classification of complications. J Endourol. 2011;25(8):1275-1280.
doi pubmed - Scholes RL, Browning L, Sztendur EM, Denehy L. Duration of anesthesia, type of surgery, respiratory co-morbidity, predicted VO2 max and smoking predict postoperative pulmonary complications after upper abdominal surgery: an observational study. Aust J Physiotherapy. 2009;55:191-198.
doi - Akman T, Binbay M, Sari E, Yuruk E, Tepeler A, Akcay M, Muslumanoglu AY, et al. Factors affecting bleeding during percutaneous nephrolithotomy: single surgeon experience. J Endourol. 2011;25(2):327-333.
doi pubmed - Cormio L, Preminger G, Saussine C, Buchholz NP, Zhang X, Walfridsson H, Gross AJ, et al. Nephrostomy in percutaneous nephrolithotomy (PCNL): does nephrostomy tube size matter? Results from the Global PCNL Study from the Clinical Research Office Endourology Society. World J Urol. 2013;31(6):1563-1568.
doi pubmed - El-Nahas AR, Shokeir AA. Percutaneous nephrolithotomy: keeping the bridge for one night. Urol Res. 2012;40(4):389-393.
doi pubmed - Abdelhafez MF, Wendt-Nordahl G, Kruck S, Mager R, Stenzl A, Knoll T, Schilling D. Minimally invasive versus conventional large-bore percutaneous nephrolithotomy in the treatment of large-sized renal calculi: Surgeon's preference? Scand J Urol. 2016;50(3):212-215.
doi pubmed - Semins MJ, Bartik L, Chew BH, Hyams ES, Humphreys M, Miller NL, Shah O, et al. Multicenter analysis of postoperative CT findings after percutaneous nephrolithotomy: defining complication rates. Urology. 2011;78(2):291-294.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.
